Why a 5-minute plan matters
Anxiety disorders are among the most common mental health conditions worldwide, yet many people do not have immediate access to professional care. Short, reproducible techniques give people tools to reduce the intensity of acute episodes while longer-term care is arranged. The goal of a 5-minute plan is simple: shift the body out of an overwhelming fight-or-flight state and give the thinking mind a chance to follow.
Understanding the difference: anxiety vs. panic
Before choosing a technique, it helps to know the difference between chronic anxiety and an acute panic attack.
Anxiety (anticipatory)
- Builds gradually and is often tied to future worries.
- Common physical signs: muscle tension, restlessness, fatigue.
- Involves cognitive areas like the prefrontal cortex — the brain’s planning center.
Panic (abrupt alarm)
- Comes on suddenly, often peaking within minutes.
- Intense physical symptoms can include racing heart, breathlessness, sweating, trembling, chest discomfort, and feelings of unreality.
- Driven by primitive alarm systems (amygdala, autonomic nervous system) and often requires immediate physiological regulation.
If symptoms resemble a medical emergency (severe chest pain, fainting, difficulty breathing that doesn’t respond to calming techniques), seek medical evaluation.
The physiological target: switch on the body’s “off” switch
Panic triggers a large sympathetic (stress) response. The fastest way out is to engage the parasympathetic system — the body’s rest-and-digest response — primarily via the vagus nerve. Practices that stabilize breathing, use strong sensory input, or provide a rapid somatic shift can stimulate vagal pathways and reduce heart rate and alarm.
Category 1 — Vagal-toning breathing (fastest, highest yield)
Breath control is the quickest method to change the body’s state because breathing directly interfaces with heart rate variability (HRV) and the autonomic nervous system.
Diaphragmatic (belly) breathing — the foundation
- Sit or lie comfortably. Place one hand on your chest and one on your belly.
- Breathe in slowly through your nose so your belly rises (not your chest).
- Exhale slowly, letting the belly fall.
- Aim for longer exhales than inhales (for example: 4 counts in, 6–8 counts out).
Practice for 1–5 minutes when you feel tension building or during an acute episode.
4-7-8 breathing (step-by-step)
- Sit upright and relax your tongue (tip touches the ridge behind the upper front teeth if comfortable).
- Exhale fully through the mouth with a soft “whoosh.”
- Close your mouth and inhale quietly through the nose for 4 seconds.
- Hold the breath for 7 seconds.
- Exhale audibly through pursed lips for 8 seconds.
Repeat 3–4 cycles. The long exhale is key — it encourages parasympathetic activation.
Box (square) breathing — steadiness under pressure
- Inhale for 4 seconds.
- Hold for 4 seconds.
- Exhale for 4 seconds.
- Pause with empty lungs for 4 seconds.
Repeat 4–6 times. This rigid rhythm reduces chaotic breathing and refocuses attention.
Category 2 — Sensory grounding & pattern interrupts
When anxiety traps attention in catastrophic loops, a powerful pattern interrupt is to redirect attention to immediate sensory facts.
5-4-3-2-1 sensory grounding
Use your five senses in descending order:
- 5 things you can see (name them).
- 4 things you can feel (texture, pressure, temperature).
- 3 things you can hear (near or far sounds).
- 2 things you can smell (or two scents you can imagine).
- 1 thing you can taste (sip water, note the flavor).
This stepwise sequence strongly reorients attention to the present moment and helps the nervous system re-calibrate.
Somatic interrupts — quick physical resets
- Cold-water splash / ice: Splashing cool water on your face or holding ice briefly activates the mammalian diving reflex and stimulates parasympathetic tone. Use cautiously if you have cardiac conditions and consult a clinician as needed.
- Discharge movement: Shake out arms and legs vigorously for 30 seconds, stomp briefly, or do a fast paced set of shoulder rolls. These actions help expel trapped activation.
Category 3 — Cognitive defusion & reframing (short mental shifts)
After the body begins to calm, short cognitive techniques reduce the emotional charge of anxious thoughts.
Naming the thought
When a fearful thought appears, label it: “I am having the thought that…,” or “Here’s the ‘what-if’ story.” That grammatical shift creates distance and weakens the thought’s command.
Leaves on a stream (visual defusion)
- Close your eyes safely or soften your gaze.
- Imagine a gentle stream with leaves floating by.
- Place each passing anxious thought on a leaf and watch it drift away.
This visualization promotes non-attachment to thoughts and takes under five minutes.
Quick guided imagery for safety
Create a vivid, sensory “safe place” in your mind (a beach, forest, or room). Spend one to three minutes noticing sights, sounds, smells, and textures. This trains the brain to shift from threat processing to calm imagery quickly.
Integrating and practicing these techniques
- Practice daily for skill acquisition. A 5-minute daily habit strengthens the link between the cue (stress) and the calm response. Over time HRV improves and resilience increases.
- Combine approaches. For example: 2 minutes of diaphragmatic breathing → 1 minute of 5-4-3-2-1 grounding → 1 minute naming technique.
- Avoid the paper bag myth. Rebreathing exhaled air is not recommended; slow, controlled breathing is safer and effective.
Safe use and when to get help
These techniques help manage acute distress but are not a substitute for clinical care. Seek professional support if: panic or anxiety is frequent, causes significant life impairment, or if symptoms include persistent chest pain, fainting, or breathing difficulty that doesn’t improve. Effective treatments exist, including psychotherapy (CBT, ACT) and medication when appropriate.
Quick 5-minute protocol you can memorize
- Sit or stand safely. Place one hand on your belly. (10 seconds)
- Do 2 cycles of diaphragmatic 4-6 breaths (60–90 seconds).
- If still activated — perform 2 rounds of 4-7-8 (3–4 cycles). (90–120 seconds)
- Do the 5-4-3-2-1 grounding sequence (60–90 seconds).
- If tension persists, shake out limbs for 30 seconds or splash cool water on face. (30 seconds)
Total: ~4–5 minutes.
Common myths & safety notes
- Myth: Panic causes fainting. Fact: Fainting is rare during panic; the nervous system usually increases heart rate and blood pressure rather than dropping them.
- Myth: Paper bags are a safe fix for hyperventilation. Fact: Rebreathing can be unsafe, especially for people with heart or respiratory issues — use slow breathing techniques instead.
Final encouragement
These practices are simple but powerful. Repetition builds automaticity: the more you practice in calm moments, the faster your nervous system will learn to settle when distress arrives. If panic remains frequent, reach out to a licensed mental health provider — help is effective and available.
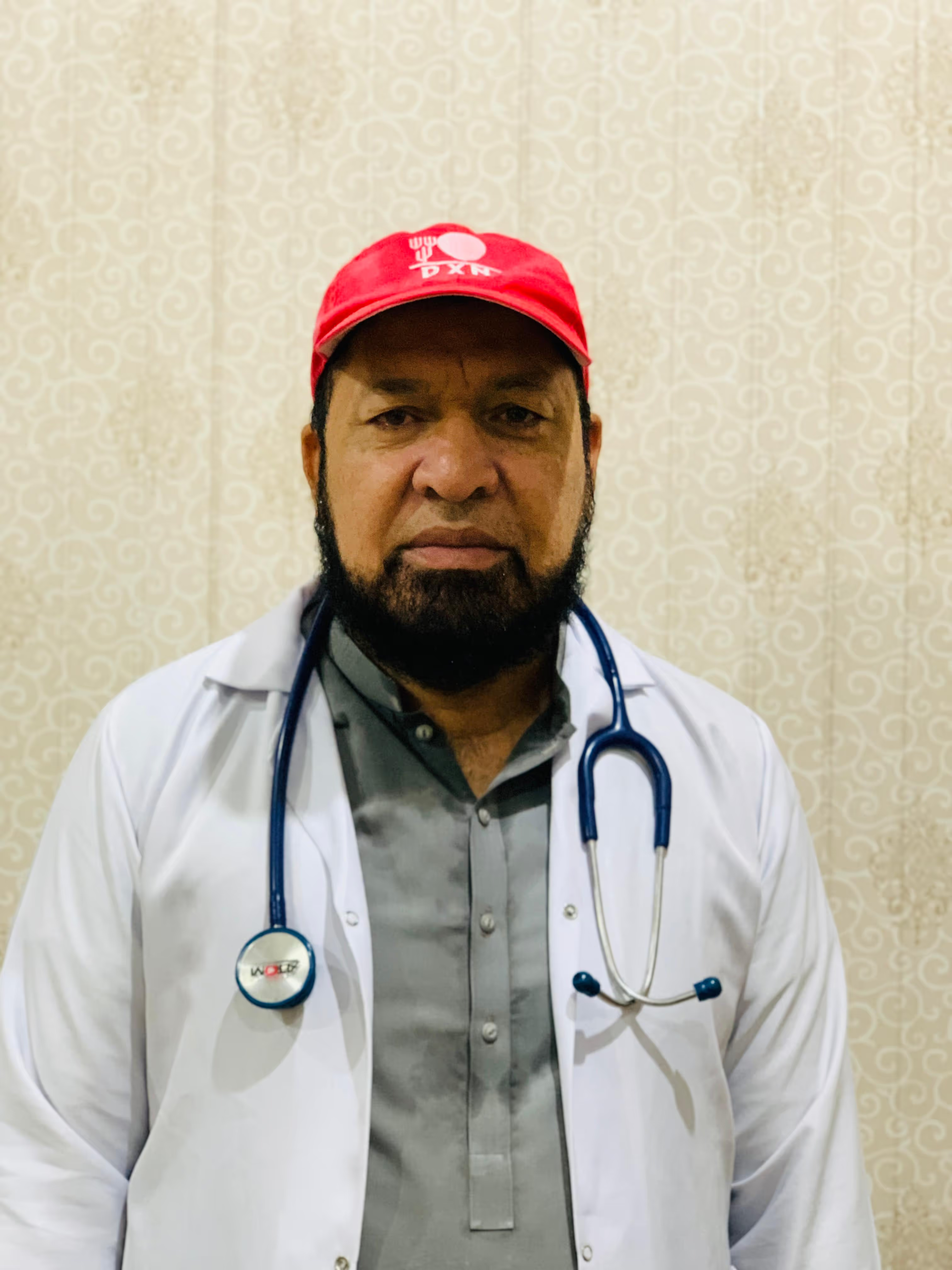
Report Author
Dr. Muhammad Iqbal